The Office of Inspector General (OIG) reported that Medicare Part D covered nearly $425 million for medications that hospices should have paid for.
Through PEPPER (Program for Evaluating Payment Patterns Electronic Report), Medicare provides hospice-specific data statistics for Medicare claims that may be at risk for improper Medicare payments. However, actionable details such as medications, patients, and dispensing pharmacies are not provided in the report, leaving hospices without key claims information.
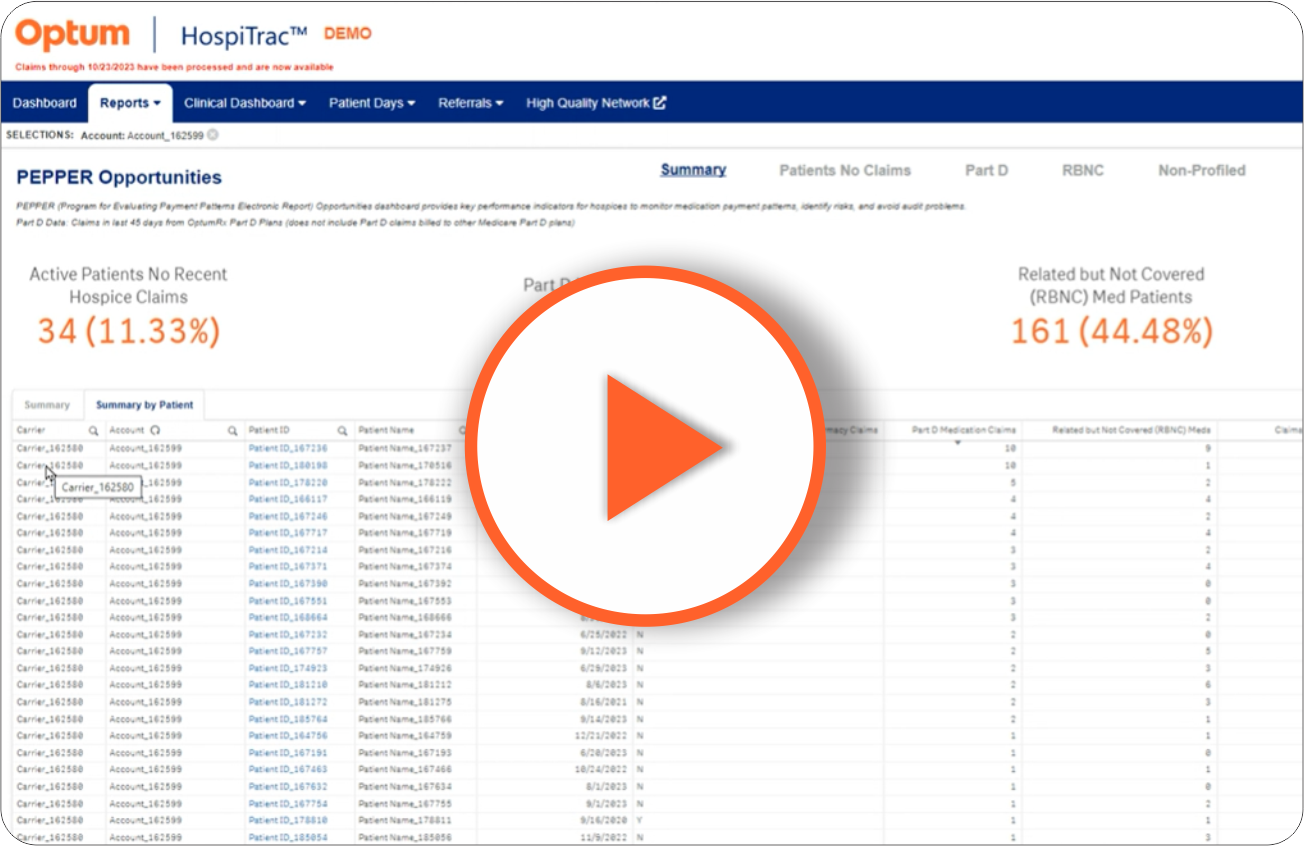
Learn how the new Optum PEPPER Dashboard can highlight actionable details that are not provided to your hospice by Medicare.
PEPPER dashboard data
Available in the Optum HospiTrac™ reporting suite, Key Performance Indicators (KPIs) summarize the user's selections at the top of the page, along with navigation within the dashboard:
| Patients without claims: Lists active patients on service at least 45 days with no pharmacy claims in the past 45 days.. |
| Part D medication claims: Provides data from Optum Rx Part D Plans with claims for active patients, occurring in the last 45 days. |
| Related but not covered (RBNC) medications: Lists medications that hospice has indicated as non-covered but may be related to the terminal prognosis. RBNC uses an algorithm to calculate relatedness probability. |
| Claims for medications not on patient profile: Lists medications with hospice-paid claims that have not yet been profiled in patient's Optum medication list. |
PEPPER dashboard demo
Imagine how a few simple clicks can provide the details your hospice needs. Watch this short video to see how easy it is to access valuable PEPPER data.
More information
Discover how your hospice can benefit from this and other Optum solutions for your hospice. Contact us to receive additional info and talk to a Optum representative.